Short commentary: 2025 Vol: 17 Issue: 1
A Rare Case of Sister Joseph Nodule in Carcinoma of Colon Diagnosed by Fine Needle Aspiration Cytology
Libni D Angel*
Department of Chemistry, Institute of Science, Banaras Hindu University, Varanasi, India
*Corresponding Author:
- Libni D Angel Department of Chemistry, Institute of Science, Banaras Hindu University, Varanasi, India
Received: 31-Jul-2024, Manuscript No. JOCPR-24-143849; Editor assigned: 02-Aug-2024, PreQC No. JOCPR-24-143849 (PQ); Reviewed: 16-Aug-2024, QC No. JOCPR-24-143849; Revised: 30-Jan-2025, Manuscript No. JOCPR-24-143849 (R); Published: 07-Jan-2025, DOI:10.37532/0975-7384.2025.17(1).230.
Citation: © 2025 Angel LD. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Umbilical skin metastasis, also known as Sister Mary Joseph nodule, is a rare manifestation of advanced malignancies, most commonly associated with gastrointestinal and gynecological cancers. Its occurrence in colon carcinoma is particularly uncommon, with limited documented cases. This report discusses a 61-year-old male with a history of mucinous carcinoma of the colon treated with hemicolectomy and chemotherapy. The patient presented two years later with a swelling on the anterior abdominal wall, later identified as a metastatic deposit near the umbilicus. Clinical examination, imaging studies and Fine-Needle Aspiration Cytology (FNAC) confirmed the malignant nature of the lesion, consistent with metastasis from colon carcinoma. Umbilical metastasis indicates advanced disease and poor prognosis, underscoring the need for comprehensive diagnostic evaluation. This case highlights the importance of recognizing such atypical presentations and their diagnostic challenges in metastatic disease.
Keywords
Sister Mary Joseph nodule; Umbilical metastasis; Colon carcinoma; Mucinous carcinoma; Metastatic deposits
Introduction
Umbilical skin metastasis, more commonly known as Sister Joseph nodules, is a rare yet clinically significant manifestation of metastatic disease. The terminology is attributed to Sister Mary Joseph Dempsey, a surgical assistant who first highlighted the importance of this metastatic presentation by publishing an article on the subject in the year 1928 [1]. These metastatic nodules are most frequently associated with primary malignancies originating in the stomach and ovary, where they are more commonly observed. However, the occurrence of such nodules in cases of carcinoma of the colon is considered to be an exceedingly rare phenomenon, thereby increasing their clinical and diagnostic interest.
The first-ever documented case of umbilical metastasis in colon cancer can be traced back to 1846, when it was initially reported by Walshe [2]. The presence of umbilical metastasis in a patient generally signifies an advanced stage of cancer progression, which is often associated with a significantly poorer prognosis and a markedly reduced survival rate [3]. This case report serves to highlight a rare and particularly intriguing instance of umbilicalmetastasis detected in a patient who had previously undergone treatment for colon carcinoma [4].
Literature Review
Clinical presentation-clinical history and findings
A 61-year-old male patient, with a previously diagnosed case of mucinous carcinoma of the colon classified as PT4N2bMx, underwent comprehensive treatment in 2019 [5]. The treatment regimen included a left hemicolectomy followed by a transverse colectomy, accompanied by 12 cycles of adjuvant chemotherapy [6]. Subsequently, in the year 2020, the patient underwent a reversal of the transverse colostomy with end-to-end anastomosis. In 2021, the patient presented with complaints of bilateral leg swelling, which had persisted for 25 days [7]. The swelling was insidious in onset and non-progressive in nature [8].
During the clinical examination, the patient’s vital signs were found to be stable [9]. However, a per-abdominal examination revealed mild tenderness localized to the right hypochondrium [10]. The physical examination also showed the presence of midline laparotomy and colostomy scars. Notably, a solid swelling was observed over the anterior abdominal wall.
To investigate further, a USG imaging of the abdomen was performed, but it did not reveal any significant abnormalities. Consequently, a PET-CT scan was conducted, which showed mildly hypermetabolic circumferential mural thickening, with the thickest segment measuring 10 mm, extending over a length of 2.5 cm and associated with luminal narrowing near the colorectal anastomosis site. Additionally, another segment of hypermetabolic circumferential mural thickening, also with a maximum thickness of 10 mm, was observed extending over a length of 5 cm, approximately 5 cm proximal to the previously noted lesion near the anastomosis site.
The scan findings also identified a moderately hypermetabolic subaortic lymph node measuring 11 × 9 mm and a faintly hypermetabolic left supraclavicular lymph node measuring 12 × 6 mm, both suspicious for metastatic involvement. Other findings included faintly hypermetabolic stranding in the left lower anterior abdominal wall, suspected to be inflammatory post-surgical changes, faintly hypermetabolic and enlarged bilateral inguinal lymph nodes likely representing reactive changes, and faintly hypermetabolic peritoneal stranding with a soft tissue density measuring 54 × 23 mm in the left iliac region, suspected to represent post-surgical alterations.
To further evaluate the solid swelling on the anterior abdominal wall, located slightly below the umbilicus, a Fine-Needle Aspiration Cytology (FNAC) was performed. During abdominal examination, the midline laparotomy and colostomy scars were reaffirmed, along with the presence of a swelling measuring 5 × 3 cm. The swelling was localized just below the umbilicus on the anterior abdominal wall.
FNAC findings: A fine needle aspiration cytology was done from the swelling over the anterior abdominal wall just below the umbilicus.
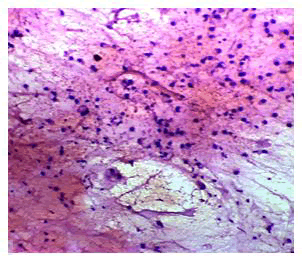
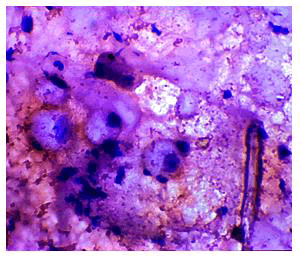
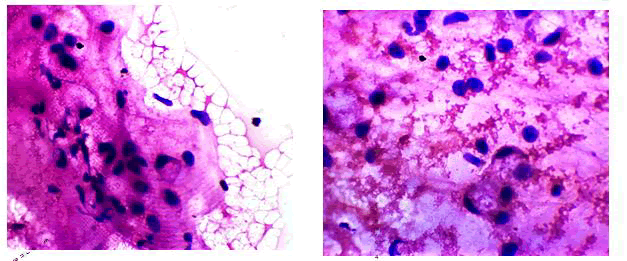
Aspirated smears showed atypical cells, some cells with signet ring cells feature hyperchromatic nuclei in a mucinous background. Impression was given as features are that of malignancy possibly from the metastatic deposit of colon (Figures 1-3).
Figure 1: Cytology smears showing 4x view of atypical cells in a mucinous background.
Figure 2: 40x magnification view showing cells with signet ring cell features.
Figure 3: 10x magnification view showing atypical cells with hyperchromatic nuclei and few with signet ring like features.
Discussion
The malignant metastatic umbilical nodule, commonly referred to as the "Sister Joseph Nodule," is a rare yet significant clinical finding. It accounts for approximately 1% to 3% of all cases of abdominal and pelvic carcinomas, making it an uncommon but notable presentation in oncology. The umbilicus is particularly vulnerable to metastatic deposits due to its unique vascular variations and developmental anomalies, which provide multiple pathways for tumor spread.
Carcinomas can metastasize to the umbilicus through various routes, including the portal venous system of the umbilical vein, regional lymph nodes, dermal lymphatics and even arterial embolization. The diverse mechanisms underscore the complexity of metastatic dissemination to this anatomical site. Comprehensive histological and cytological evaluations of all umbilical lesions are essential for determining their nature. These assessments not only help in confirming malignancy but are also critical in identifying the primary tumor source when the lesion is diagnosed as metastatic.
Umbilical nodules are clinically intriguing as they can present either as benign or malignant growths. Among malignant cases, these nodules may be classified as primary or secondary metastatic tumors. On the other hand, benign umbilical nodules encompass a variety of conditions such as endometriosis, melanocytic nevi, fibroepithelial papillomas, keloids, myxomas, abscesses, umbilical hernias, dermatofibromas, seborrheic keratosis and pilonidal sinuses. This diverse range of differential diagnoses emphasizes the need for thorough diagnostic workups to accurately classify and manage umbilical lesions.
Conclusion
A variety of cutaneous tumors that arise on or around the umbilical region have the potential to be misdiagnosed as the Sister Mary Joseph nodule, which is a metastatic umbilical lesion associated with advanced malignancies. Differentiating between these tumors is essential, as they may include both benign and malignant conditions that mimic the appearance of metastatic nodules. The clinical and cytological findings presented in this study provide valuable insights and play a crucial role in aiding accurate diagnosis by highlighting distinctive features of the Sister Mary Joseph nodule compared to other umbilical lesions.
Following the confirmation of the diagnosis, the patient was referred to a palliative care center to receive further management. This decision underscores the advanced stage of the disease and the need to focus on improving the quality of life and providing symptom relief. Comprehensive palliative care is an integral part of managing such cases, ensuring that the patient receives holistic and supportive treatment tailored to their individual needs.
References
- Huang CW, et al. J Colorectal Surg Soc Repub China. 2020;31(4):221-228.
- Wu YY, et al. Chin J Cancer. 2010;29(2):239-241.
[Crossref] [Google Scholar] [PubMed]
- Akhtar K, et al. Clin Pract. 2011;1(1):9-10.
[Crossref] [Google Scholar] [PubMed]
- Urbano FL. Hosp Physician. 2001;37(5):33-44.
- Wronski M, et al. J Ultrasound Med. 2014;33(3):531-534.
[Crossref] [Google Scholar] [PubMed]
- Powell FC, et al. J Am Acad Dermatol. 1984;10(4):610-615.
[Crossref] [Google Scholar] [PubMed]
- Al-Mashat F, et al. Indian J Cancer. 2010;47(1):65.
[Crossref] [Google Scholar] [PubMed]
- Gupta RK, et al. Diagn Cytopathol. 1994;10(2):126-129.
[Crossref] [Google Scholar] [PubMed]
- Chalya PL, et al. World J Surg Oncol. 2013;11:1-6.
[Crossref] [Google Scholar] [PubMed]
- Larbcharoensub N, et al. Mol Clin Oncol. 2016;5(5):557-561.
[Crossref] [Google Scholar] [PubMed]